Abstract
Background: Black race and Hispanic ethnicity have been associated with inferior outcomes in prior studies of acute myeloid leukemia (AML). Understanding potential mitigating or contributing factors, including social determinants of health (SDOH), for disparities in outcome is paramount to improving the care of these vulnerable populations. Levine Cancer Institute (LCI) has a unique care delivery model incorporating health and social services, including specialized oncology nurse navigation (ONN), and serves greater than 19,000 new patients (pts) per year from a large metropolitan community and extensive outlying rural areas. We examined potential health disparities and contributing factors among AML pts.
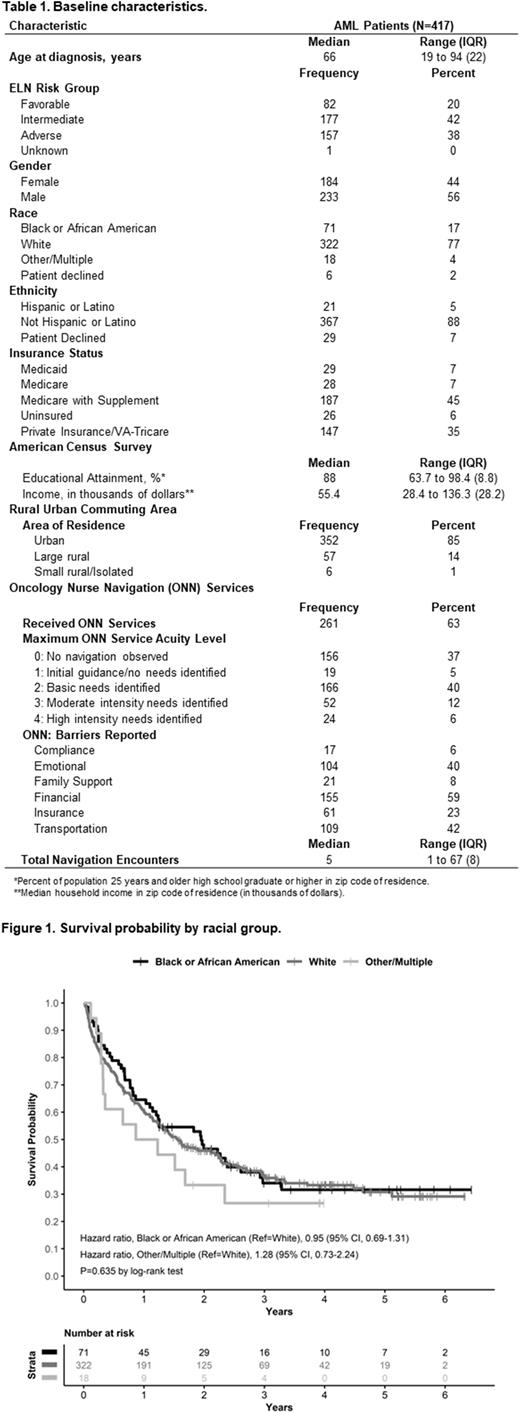
Methods: Adult AML pts who presented to LCI between 12/2015 and 12/2020 were included. Demographics, disease characteristics, insurance coverage, ONN metrics, ONN-identified psychosocial barriers, census tract data, Rural-Urban Commuting Areas (RUCA), and survival outcomes were collected and included in this analysis. Race and ethnicity were self-reported. European LeukemiaNet (ELN) criteria were used to risk stratify patients. Descriptive statistics were used to summarize the study population. The associations between overall survival (OS) and pt and disease characteristics, insurance status, race, ethnicity, census tract data, and ONN services were investigated. OS was defined as the time from diagnosis to death from any cause, with surviving subjects censored at the time of last follow-up. Kaplan-Meier method and log-rank testing for univariate comparisons were used to determine probabilities of OS. Multivariable analysis (MVA) was performed using a Cox proportional hazards regression model.
Results: There were 417 AML pts with available baseline characteristics included and summarized in Table 1. Most pts were Non-Hispanic White (77%). There was no significant difference in OS among racial groups (Figure 1). A plurality had Medicare with Supplement (45%), followed by private insurance (35%). Although a majority of pts resided in an urban area (85%), 14% of pts came from large rural areas. For the entire cohort, median OS was 18.8 months with a median follow up of 16.9 months. ONN services were provided for 261 (63%) pts. ONN identified obstacles to care, with financial barriers reported in 155 (59%) pts, followed by transportation issues in 109 (42%), and emotional challenges in 104 (40%). ONN identified insurance barriers in 23% of pts. In MVA, older age (Hazard Ratio [HR] 1.18, P<0.001), intermediate (HR 2.49, P<0.001) or adverse ELN risk (HR 4.12, P<0.001), and no receipt of ONN (HR 1.69, P<0.001) were associated with inferior OS. To further examine potential disparities in our population, a separate analysis was performed on the navigated cohort (N=261). There was no difference in receipt of ONN across racial or ethnic groups. Older age (HR 1.2, P<0.001) and intermediate (HR 1.74, P<0.001) and adverse risk status (HR 3.51, P<0.001) remained associated with inferior OS. In the navigated cohort, higher total number of navigation encounters was associated with improved OS (HR 0.94, P=0.007).
Conclusions: In contrast to prior studies, self-reported Black/African American race or Hispanic ethnicity was not associated with inferior survival in a large and diverse cohort of AML pts from urban and large rural areas. With several factors reflective of SDOH described, none were associated with OS. For the entire cohort, MVA revealed that age, ELN risk, and absence of ONN were associated with inferior OS. Importantly, there was no difference between percentages of racial groups receiving ONN services; among the navigated cohort, racial or ethnic disparities in OS were not identified. Regarding insurance, having Medicare or Medicare with Supplement did appear significant in univariable analysis, but in MVA insurance status was shown to be confounded by age. As ONN interacts with and seeks to help address many SDOH, the association between ONN and better OS may suggest a potential mitigating strategy to address previously reported disparities in AML pts.
Disclosures
Chojecki:Servier: Consultancy, Membership on an entity's Board of Directors or advisory committees; Incyte: Research Funding; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees. Patel:Bristol Myers Squibb: Research Funding; Clarified Precision Medicine: Consultancy; VieCure: Consultancy. Symanowski:Immatics: Consultancy; Eli Lilly & Co.: Consultancy; Camarus: Consultancy; CARsgen: Consultancy. Grunwald:Genetech/Roche, Incyte Corporation, Janssen: Research Funding; Medtronic: Current equity holder in private company; Daiichi Sankyo, Gamida Cell, Gilead Sciences, Incyte Corporation, Invitae, Karius, Novartis, Ono Pharmaceutical, Pfizer, Pharmacosmos, Premier, Sierra Oncology, Stemline Therapeutics: Consultancy; AbbVie, Agios/Servier, Amgen, Astellas Pharma, Blueprint Medicines, Bristol Myers Squibb, Cardinal Health, CTI BioPharma, Daiichi Sankyo, Gamida Cell, Gilead Sciences, Incyte Corporation, Invitae, Karius, Novartis, Ono Pharmaceuticals, Pfizer, ,: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal